Insurance Coverage Assistance
Some insurance companies realize that removal of breast implants can be medically necessary for women’s health to improve and will offer policies to cover the removal surgery. Obtain a copy of your insurance policy and review it to see if they are likely to pay for the removal. Generally, the insurance criteria focus on capsular contractures, ruptures, infections, and chronic breast pain. Some insurances have added coverage for removal of Allergan Biocell textured breast implants and tissue expanders after the global recall (Class I recall in the US) due to risks of BIA-ALCL. Accompany one or more medical necessity letter(s) with the specific insurance codes, some are listed below. See Sample Medical Necessity Letter and Private Insurance Help by the National Center for Health Research. The process of getting approved may require tenacity and perseverance, if you get denied the first time repeal as many times as necessary. Do not get discouraged, one woman reapplied three times and then was approved. The key with insurance is really to be persistent. If you have exhausted the appeals procedure, you can file a complaint with the state insurance commissioner. Finally, if all else fails, you can hire an attorney to write your insurance a letter for failing to cover a medically necessary procedure.
Insurance companies that have covered women:
- Aetna – Breast implant Removal
- Aultcare: OH
- Blue Cross Blue Shield: AZ, FL (covered 90%), MI, MN, NM, NY, OK, WA, CA.
- BCBS AZ covers explants as of February 2019. Here is the specific content that was changed: “Removal of a breast implant for any non-cosmetic, medical complication or consequence, whether immediate or delayed, that arises from a prior cosmetic breast implant is considered medically necessary and eligible for coverage.”
- BCBS CA PPO, doctor submitted notes of exam to insurance and discussed chest and breast pain.
- BCBS MN covered an explant of a woman with capsular contracture (Baker Grade IV in one breast and II in the other).
- Community Care of OK
- Kaiser
- Medi-Cal
- Moda: WA
- SelectHealth insurance in Utah (Select Med plan)
- Helped cover partial costs of explant for a woman. She did not have rupture or capsular contracture but she did have pain.
- Tricare: CO, OK (Tricare Standard)
- UCare: MN.
- Patient was able to have the explant covered, did not have capsular contracture but did complain of pain.
- United Healthcare: Coverage Determination, now covers explants for Allergan recalled textured breast implants (August 2019 update).
- Tufts Health Direct through Health Connector in MA covers removal if there is a rupture or one has been diagnosed with an autoimmune disorder.
- Provincial Health (Alberta Health Care, Canada)
- Cigna: CO, TN, UT
- As of January 15, 2020, Cigna updated its Breast Implant Removal (0048) coverage criteria by adding removal of Allergan Biocell textured breast implants and tissue expanders.
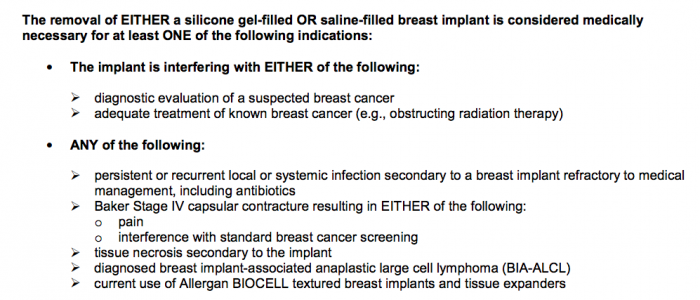
- See page 2 of Cigna Medical Coverage Policy 0048 for coverage criteria:
Please note that policies vary by state and coverage depends on your specific medical circumstances.
Steps and Letters to Help Get Insurance to Cover Explant
BII Explant Insurance – Google Drive includes all the steps and letters a woman did to help get her insurance to cover explant.
Kantor & Kantor – Explants Denied by Insurance Claims:
Kantor & Kantor law firm in California was able to get an explant insurance denial overturned. See Coverage for Breast Explant Surgery Was Denied – Kantor & Kantor Stepped In and Got the Denial Overturned (June 2019).
They are now interested to speak to women who have had to pay out-of-pocket for explant and have had explant insurance denials from: BCBS California, BCBS of Illinois, BCBS of Montana, BCBS of New Mexico, BCBS of Oklahoma, and BCBS of Texas. Please contact attorney Cari Schwartz if you meet these case criteria and are interested in filing a lawsuit, her contact number is (818) 886-2625. Schwartz is working on bring a class-action lawsuit against insurance companies that deny explant coverage.
Mastectomy Cases
“If your implants were put in after a mastectomy and your doctor believes that removing your implants is “medically necessary,” then your health insurance is legally obligated to cover your breast implant removal. Click here to learn more about your rights under the Women’s Health and Cancer Rights Act of 1998 (WHCRA).”1
Medicare and Medicaid
Medicare and Medicaid will often cover the costs of breast implant removal. If you have applied or are on Social Security Disability Insurance (SSD/SSDI) or Supplemental Security Income (SSI) you may be able to have the costs of explantation covered by them. The problem with Medicare is that they do not preapprove anything. Your local Medicare or Medicaid office is likely to have a list of plastic surgeons that accept their coverage. Ensure they will remove the implants with full capsule removal, via en bloc or total capsulectomy.
According to Centers for Medicare & Medicaid Services (CMS), which is the government program that regulates Medicare services, Medicare authorizes the removal of breast implants for the following reasons:
“Removal or revision of a breast implant whether placed for reconstructive or cosmetic reasons, is considered medically necessary when it is removed for one of the following reasons:
-
- Mechanical complication of breast prosthesis; including rupture or failed implant, and/or implant extrusion.
- Infection or inflammatory reaction due to a breast prosthesis; including infected breast implant, or rejection of breast implants.
- Other complication of internal breast implant; including siliconoma, granuloma, interference with diagnosis of breast cancer, and/or painful capsular contracture with disfigurement.”
Source: Cms.gov Medicare Coverage Database (LCD L39051)
See: Will Medicare Pay to Remove My Breast Implants? by the National Center for Health Research
National Center for Health Research | Breast Implant Information Organization
Update:
“We are happy to announce that we are resuming insurance coverage assistance for women who need help getting insurance to pay for removal. Due to the importance of our work and the hundreds of women we have been able to help over these past few years, we have secured new funding to continue our project so that we can assist hundreds of more women in navigating the health insurance process for breast implant removal.
The National Center for Health Research is a nonprofit organization assisting women who seek health insurance coverage or Medicare coverage for the medically necessary removal of their breast implants. They can be contacted by email at [email protected]. Sample of a message women have received from them is: “If you are having problems with your breast implants, we want to help you succeed in getting health insurance coverage so you can get them removed as soon as possible. Please reply if you’d like our help!”
The Breast Implant Information is sponsored by the National Center for Health Research. If you would like their assistance with the insurance process, please take this short survey, and they should be in touch with you. Or you can also contact them at [email protected] or (844) 295-2212. They recommend taking the following steps and can assist you with them:
- Send them a copy of your insurance policy so they can review it.
- Get a consultation with plastic surgeon who is experienced in explant.
- Ask your surgeon/doctor if they can write a letter of medical necessity and help you file a claim.
- File your claim with the relevant medical documents, medical necessity letter, and insurance codes.
- If you get approved, congratulations! If you get denied, appeal as many times as necessary.
Resources:
Sample Letters of Medical Necessity for Insurance Coverage of Explantation
Insurance Codes:
CPT
19371-50 – Periprosthetic capsulectomy, breast – the 50 modifier is for – Bilateral Procedure
ICD 10
T85.49XA – Other mechanical complication of breast prosthesis and implant, initial encounter
T85.79XA – Infection and inflammatory reaction due to other internal prosthetic devices, implants and grafts
T85.848A – Pain due to internal prosthetic devices, implants and grafts
T85.44XA – Contracture of Breast Prosthesis
T85.43XA – Rupture of Breast Prosthesis
N64.81 – Breast Ptosis
N64.4 – Mastodynia
BIA-ALCL
ASPS Insurance Coverage for Third-Party Payers – BIA-ALCL. It addresses symptoms, insurance issues, insurance codes, imaging for evaluating symptoms, and more.
BIA-ALCL Diagnosis (ICD-10)
C84.79 Anaplastic large cell lymphoma, ALK-negative, extranodal, solid organ sites N63 Unspecified lump in breast, nodule, mass, or swelling of the breast
R59.9 Enlarged lymph node
N64.89 Other specified disorders of breast
BIA-ALCL Procedure (CPT)
10022 Fine needle aspiration with imaging guidance 19101 Breast biopsy, open, incisional
19260 Excision of chest wall tumor
19328 Removal intact mammary implant
19371 Breast periprosthetic capsulectomy
38525 Biopsy/excisions, lymph node; open or deep axillary node
Sign Petition:
FDA & CDC – Develop a medical code for sick women suffering from breast implants
An ICD-10 diagnosis code is currently not available. It would help women to file a claim with insurance companies to help with explant surgery costs. This petition is sponsored by the Global Patient Advocacy Coalition (GPAC).
Rachel Brummert was a Consumer Representative at the FDA hearing on breast implants in March 2019. She spoke to MedTruth about the need for ICD insurance codes for breast implant illness:
“I was the FDA Consumer Representative at the March 25-26 2019 FDA hearing. I saw the evidence from both FDA and device makers and heard testimony from over 80 harmed patients. There is a dire need for changes to protect patients. FDA and other agencies are dragging their feet in implementing any of them and I will use my voice and expertise to do right by patients.”
International:
South Africa Explant Insurance Coverage:
Medihelp Necesse Package covered a woman’s explant in full when she had a breast ultrasound and it confirmed that the implants leaked, as a note it took three ultrasounds to finally detect the leak.
Momentum covered most of another woman’s explant when she had her surgeon write them a letter emphasizing two large lumps.
Additionally, the Bone and Breast Care Centre comes recommended for specializing in breast scans and reports. See above for codes to submit to insurance, South Africa uses some of the same ones as the U.S.
UK Explant Insurance Coverage:
Some women have had success with having the NHS cover their explant. One woman went to her doctor and explained the pain and discomfort she was in and was referred to a hospital breast clinic where she then had her explant. In consideration of this option, please ensure full capsule removal.
Netherlands Explant Insurance Coverage:
Zorginstituut Nederland sent a memo to all health insurance companies in May 2018. They state that when a woman has health issues that do not go away with treatment that explant should be paid through insurance. Therefore, if you can show a history of doctor visits and have systemic symptoms, explant should be covered.
Canada Explant Insurance Coverage:
Allergan Recalled Textured Breast Implants – MSP Funded Explant Surgery in BC, Canada
In B.C., public health insurance is called the Medical Services Plan (MSP). The MSP has decided to fund explant surgery for patients with the recalled Allergan textured breast implants. If you live in B.C. and have the recalled Allergan implants you can see your primary doctor and have a discussion about explant and MSP funding it. Hopefully other provinces’ public health systems follow B.C.’s lead.
German Woman Wins Disability from Silicone Breast Implants:
In May 2020, a woman in Germany won a two year case for disability from breast implant illness. She was initially denied disability so she started a lawsuit.
In November 2019, the court assigned a psychiatrist who told her breast implant illness did not exist and said her illness was caused by social media.
The woman did not accept this decision and applied for a second review. In February 2020, she was assigned an environmental medicine specialist, Dr. med. Martin Schata in Düsseldorf, who ran extensive blood work. In May 2020, she got her new decision:
Chronic inflammation in multiple organs, chronic fatigue as a result of immune response to silicone breast implants. Disabled 60%.
Visit the German BII website (Krank Durch BrustImplantate) and German FB group (Krank Durch Brustimplantate – Breast Implant Illness DE) for more information. The woman in the lawsuit is the founder of the first German BII FB group, mentioned above.
Separate from the court case but relevant to the matter, she found a Germany lab called CellTrend that is doing a study on the harm of breast implants to the immune system. Their test for this is called POTS Diagnostic and costs around €467.
______
Insurance companies would save on years or decades of unnecessary medical costs by recognizing the necessity of explant surgery as a cost effective protocol to prevent further systemic illness.
It’s now 2023 and am hoping a few women were successful with BCBS-TX! I am in such pain in my right breast, have Grade IV Capsular Contracture, and often can barely use my hand to write and the numbness is a grave concern. Exhaustion is the order of the day and have no life outside of work, as a result. Working out, doing yoga, sleeping on my stomach, is impossible. Need a plastic surgeon in NYC who is not a butcher. Need to get these out even if going into debt is the answer. This is not living. Any assistance would be greatly appreciated. Please email me: k.dallett@gmail Thank you!
I am looking for an explant Dr in Atlanta. Anyone know of one? I have BCBS. ANy tips>
Hello I am in Maryland I work for the Judiciary and my insurance is BCBS i am not sure if they will cover the removal but I need it in order to keep living I am in chronical pains suffering in desperate need of help.
My contact
[email protected]
I know my breast are infected and it’s fungus from mold and I take everything I can to keep it killed but it never is enough it’s a rose fungus and it’s growing in my breast I need help 58 year old disabled grandmother of 6
Does anyone here have Tricare insurance or heard of someone getting the Explant covered by Tricare? I would like to know if you got covered, how did you do it? I have been denied 3 times and I am just so sick. I have been sick since the implants were placed in the 90’s and only getting worse. Here recently, I’m even having difficulty walking and the pain is just unbearable. Any suggestions or guidance would be greatly appreciated!
Thank you! XOXO
Hi Mar Davis,
My name is Monique and I’m going to have as consultant with a surgeon in January for explant. My Dr just pit a referral into Tricare. Have you had any luck with them yet?
Helllo Monique,
Was wondering if you had any luck with Tricare? I’m in such pain and need to find a way to have my implants remove.
Hi!! Another Tricare patient here. Any luck ladies?
Hello! Just curious if this was ever approved? I also have TRICARE, was denied for my pre authorization (ruptured silicone implant) and recently submit an appeal.
Thanks in advance for any information:)
Does anyone have any guidance for choosing a surgeon for explantation. Everyone I search for suggests replacing implants. I do not want replacements, but I am concerned about where to go to have the explantation removing capsule and all without being left butchered. Any guidance would be deeply appreciated. Last, does anyone know if breast implant illness qualifies for Social Security Disability.
Hi Tina,
Did you have the Susan’s are you happy with the outcome. Have your symptoms gone away?
Implant’s not Susan.
Yes fatty tissue was want implants removed
Get them removed. Im going to Colorado on april 15th for consultation for explant. Until you get them out it will keep destroying your body. Go to youtube and type in my implants made me sick there is plenty of videos and information on this.
What surgeon are you consulting with in CO?
What surgeon are you seeing in Colorado??
Are you able to share the name of the physician you consulted with in CO?
Does anyone have Mentor smooth saline implants? I have 6 autoimmune diseases, being born with tubular breasts deformation I got impants to help the look. 2005. Now I am so weak my pain is awful. I need help yall please
I have mentor smooth saline. I have many symptoms that are debilitating. Doctors listened until I connected the dots and started suggesting that my symptoms might be related to the implants. My health is declining, I have no diagnosis, doctors categorically refuse to consider that the implants could be the cause.
I would love to chat I am on Facebook are you crystal carr please lady we can make this happen together, I
don’t know how but I have to my life depending on it.
I don’t know how either, but I would like to work together with everyone and anyone so together we may get this done. I’m slowly and painfully withering away and I want take my life back. Let me know.
This is happing to me I have allegan smooth silicone and I think I will die if I do t get help.
I have Medicaid and am going to begin the due process for explant. Does anyone know if this procedure has ever been covered by Medicaid? Have had saline implants for 18 years now and have just about all the symptoms on a list I recently obtained. I am now 50 years old and feel like Im 70 due to all the accumulating illnesses throughout the years since I had my augmentation; all these symptoms have pregressively worsened. I used to be very sports inclined and physically active 6 out of 7 days of the week. I cant even get out of bed without feeling pain in every single joint in my body and the symptoms go on and on and on… I just want to feel healthy and happy again. Wish me luck 🙏
Hi Liza! I feel like you were inside my head when you wrote that! I, too, have had my saline implants for 18 years now with accumulating symptoms throughout the years. I also feel like a 70 year old woman inside of a 40 year old body. I used to be so active myself and now I barely have the energy to even type this out. I’ve gone from being a total social butterfly, to more of a hermit who just wants to be home laying In bed at all times. I haven’t been myself for at least 3 years now. It has definitely interfered with my daily living and my ability to be a good, hands-on parent to my 3 kids. I feel defeated on the daily.
Hi Liza and Jamie! SAME!!! I feel absolutely decrepit! I too USED to be very social, high energy, active and athletic. Now I go to work, I come home, I sleep and start over the next day. I am an only parent of 4 now teenagers who haven’t had a mom for 6 years plus. My symptoms began immediately but were small enough to dismiss and attribute to something else. As they became greater in number and severity, I still thought that I had a rare tropical disease, or a brain/pituitary tumor. I have had 2 head and neck MRI’s w/ and w/o contract, 2 ct sinus ct scans (stupid crazy amount of radiation), rheumotology work up, both reproductive (specialist) and garden variety endocrine work ups, ENT work up, heptology work up, neurology work up w/ EMG and punch biopsies, derm and biopsies on rash, tests for lyme’s, babesiosis, tons of blood work, upper and lower GI, environmental and chemical allergy testing (w/ interesting results). Feels foolhardy to go into something as invasive as enbloc removal without a physicians blessing and confirming diagnostics. It is my only option and no clue how I am going to pay for it. I want my health and my life back.
Hi Penny, how are you feeling now that you had the explant surgery? Did your symptoms go away! I to have had mine for 18 years and was sick 6 months after surgery. I am 46 know and feel like I am 80. All I do is work and sleep. This is no way to live.
I saw my primary doctor yesterday and he wasn’t very optimistic that my systems would go away after explant.
Did you get approved by Medicaid for your removal?
I recently received notification from Medicare that it will pay to have the deformity resulting from my explantation fixed, provided I have the surgery prior to 6.3.19 and do not have silicone implants used as part of this correction. I currently have tenderness in both breasts, one is lower than the other, and both are flat on top. They are too painful for me to wear a bra. I have no intention of having any implants. I have misplaced the Medicare notification. If you have it, could you please email me an attached copy to [email protected] with explantation disfigurement on the subject line? Medicare told me yesterday it will do what the notice says, but refused to send me another copy. Both implants were explanted due to medical necessity: capsular contraction, pain and rupture as confirmed via MRI. Subsequent pathology confirmed extruding silicone. They were implanted in 1979 and I was assured they were saline. They were explanted in 2015. Medicare paid for the explantation.
I got implants in 2002 recently had a mammogram due to a lump. Months later i notice a significant decrease in the size of my left breast, well it was confirmed I have a ruptured saline implant!I want them out but I’m a single mom now and can not afford the removal cost! I have Medicaid through the state, does anyone know what I can do or if Medicaid will cover cost of removal?? My health is also getting worse. Fatigue, depression , weight issues , body aches.. the list goes on.. help!!
Hello Lena, I am a 48 years old and had saline implants put in ,in 1997 so they are super old and hard. They are painful to touch and I also have Medicaid thru the state of TN (Bluecare ) I desperately need mine out as well and have been turned down by a really jerk of a doctor. Making me feel like a piece of crap because I was trying to get the state to pay for it. If you find a way please let me know! I feel so crappy all the time ,I know 100% I have breastimplant illness.
Does anyone know how to or what to do to have Cigna HMO California cover explant? I am 27 years old and I feel like my life and health is deteriorating. I used to be so healthy.
Hi Stephanie
Did you ever figure out if Cigna covered the explant?
I’m trying to call, but the call itself is longer then my lunch break. Also did you see a PS or an internist? I made a list of 30+ issues I’ve gotten over the years and hate to admit they are all from having implants. Any ideas?
Thanks
I found out today that I have a rupture in both breasts because there is silicone in both my lymph nodes on both sides, including a large silicone granuloma on the right breast (I felt the lump on Satuday and fearing it was cancer had a mammogram and ultrasound today where they saw it all). Per my research on your site I want to go to Dr. Chun in Newport Beach CA or Dr. Huang in Denver as I’m in Albuquerque, NM and you don’t have anyone listed here. But you do say BCBS of NM has covered people in the past and that’s my insurance so that’s hopeful! Thank you for such a great site!
What symptoms where you having? I have started to have acute breast pain in one breast only associated with some numbness, implant looks flat from up top and small lump on side of breast, my plastic surgeon says is probably “cystic fibroma” which I never had till a week ago.
Does Medicare cover explantation?
Hi Sandy,
According to Centers for Medicare & Medicaid Services (CMS), which is the government program that regulates Medicare services, Medicare authorizes the removal of breast implants for the following reasons:
2. Removal of BREAST IMPLANTs
For a patient who has had an implant(s) placed for reconstructive or cosmetic purposes, Medicare considers treatment of any one or more of the following conditions to be medically necessary:
•Broken or failed implant
•Infection
•Implant extrusion
•Siliconoma or granuloma
•Interference with diagnosis of breast cancer
•Painful capsular contracture with disfigurement
Source: https://www.cms.gov/medicare-coverage-database/details/lcd-details.aspx?LCDId=35163&ver=13&SearchType=Advanced&CoverageSelection=Local&ArticleType=SAD%7cEd&PolicyType=Both&s=6&KeyWord=breast+implant&KeyWordLookUp=Doc&KeyWordSearchType=Exact&kq=true&bc=IAAAACAAAAAA&
I was denied by BCBSTX and have Baker IV capsular contracture. I am appealing and am so frustrated as this surgery is medically necessary.
Good luck; they denied me as well. Would love to get a class action suit going against BCBSTX.
Same here…..BCBS of Illinois, but I live in Texas. Have been denied twice with both ruptured and capsules Baker IV.
I am about to have explant surgery with bc of IL … did you have any luck with appeals ????
Good luck; they denied as well.
I have just about every issue Norma has. Went to sergeon and I have a capsulary contractors. Being confirmed with MRI. My life is like I can’t move, think straight, just walking wear me out. And it all started when my right siclone implant started felling funny, lumpy and sticking out that you can see it with naked eye. I’ve had breast cancer double mastectomy and many reconstruction surges due to a butcher of a sergeon the 1st time. I’ve been going to specialist that have done wonders, but also has taken years to try and fix a botched job
So Dr to me today we have to start over skin is so thin
So after insurance i will owe 42,000.00. Is there any finical help of any kind out there???
Anyone have Cigna in NC
I had my silicone implants removed on October 23, 2017 after 40 years. One of them was ruptured and the other one was intact. I would like to get reimbursed for my surgery and am unsure how to start the process. I would also like to submit a claim for the class action suits that were filed with a deadline of 2014. The surgeon who did the implant is retired and although the office is still in practice they do not keep records this old. I have written a letter to the hospital where I had the implants put in asking for any records but again they do not keep records this old. I have Medicare insurance as well as Blue Cross Blue Shield. After reading through some of these comments I think the first thing is to get a letter from the surgeon stating that the surgery was a medical necessity? Thanking anyone in advance for guidance.
HI Karen, looking thru old posts. I have a similar situation. Did you ever get any assistance? Thank you
I also have Kaier through Covered California. My implants were placed in 2006 the implants are covered under warranty but the procedure to replace is not . I have had several health issues with the biggest one being constant itching and breaking out in rash under the left breast . It has been noted as capsular infracture ( deflation or rupture ) along with this came the anxiety which took me off my job and I am currently on SDI since May 2017 but also off and on for about 5 years . Then I was in an accident , the airbag deployed and had made my health even worse . I am going to contact Kaiser which has a specialist to handle the procedure. I will get you the quote and send to the Implants removal assistance program
I have kaiser and would be interested in knowing how this was handled through them
OMG! Iam having the same issues with my implants.
Geez! I have them plus Medicare because of disability.
Thanks for mentioning the program of the National Center for Health Research, which has helped about 100 women get insurance coverage for implant removal in the past year+. However, you have listed my name and Farzana’s, and neither is the correct name to list as the current contact person. Please change to suggest they contact Megan at [email protected]. And please let me know how to get in touch with the person in charge of this website, because I’d like to touch base. Thank you!
Thank you Diana, I have made that change as suggested. This website can be reached by comment or email ([email protected]), your feedback is warmly welcomed.
I had saline breast implants in 1995. I was 30 years old and had no health issues. By 1997, I was sick. Was diagnosed with fibromyalgia in 1999. I am now 52 years old. I’ve been diagnosed with stiff persons syndrome,neurothapy, gastroparesis, auto immune disease, depression,anxiety, and the list goes on and on. I see specialists constantly, have to take a handful of meds daily, and receive IVG infusions 4x monthly. I’ve lost 75lbs since last year and cannot afford to lose anymore. My life has become a nightmare and I am absolutely convinced that this all started with my implants. I’m on SSA disability now because I can’t work. I have bcbs through my husband’s employer. They will not cover the explant. I don’t know where to turn, and my body continues to break down. I’m trying to bounce back from double pneumonia as I write this. Any advice at all would be so appreciated. I’m truly afraid.
Omg! Same here! I’m so sick right now and don’t have a surgeon lined up! I’m afraid too! I feel like I’m going to die!
Norma Jean, reading your illnesses souplike I am reading my biography. My first set of implants were in 1997. They ruptured in 2004. I got the second the same year. I haven’t been the same since. Started getting sick shortly after. Any and everything, that couldn’t be explained. Depression, anxiety, mood swings, bi-polar outbreaks, nausea all the time. Weight issues, either sleeping all the time or not at all. Memory issues. Joint problems, tremors, you name I have I have. I want them out. I just turned 50 in June and I just want them out
hi Norma Jean I also am on ssi disability because I haven’t been able to work since 2009. my husband also has blue cross through his employment, I was wondering about your case. were you ever able to and if so how you went about it to have blue cross cover your implant extraction
Has anyone had any experience dealing with Medicare ??
I was just denied from BCBS for implant removal. I hv baker 4 capsular contracture, dr did write a letter stating medically necessary.
Same here Julie, I also have a list of other health problems and both implants are ruptured. I have been denied twice!
I’m so sorry to hear that! I have BCBS and am waiting for them to approve or deny my pre-approval for Explant due to grade 4 Capsular Contracture and a rupture. Did they give you a reason for denial?
My doctor thinks that I will be denied too even though he states it is medically necessary, and I am in a lot of pain.