Ruptured Silicone Breast Implants
Scientific Articles:
Silicone migration to the contralateral axillary lymph nodes and breast after highly cohesive silicone gel implant failure: a case report (2009). Link.
- Silicone gel entering the lymphatics, either through overt implant rupture or slow leakage across the intact outer shell, can result in regional migration to the draining lymph node basins.
- Migration of silicone is not always limited to the corresponding axillary lymph nodes and spread to the internal mammary and inguinal nodes as well as the abdominal wall and lower back have all been reported in the literature
Lipogranulomatosis and hypersplenism induced by ruptured silicone breast implants (2013). Link.
Doctors and patients should be aware of the potential of disseminated silicone driving systemic clinical syndromes.
Silicone-mediated toxicity with distant tissue lipogranumolatosis is a feature of both silent and symptomatic implant ruptures.
An association of silicone-gel breast implant rupture and fibromyalgia (2002). Link.
Silicone gel breast implant rupture, extra capsular silicone, and health status in a population of women (2001). Link
Where there’s smoke there’s fire: The silicone breast implant controversy continues to flicker: A new disease that needs to be defined (2003). Link.
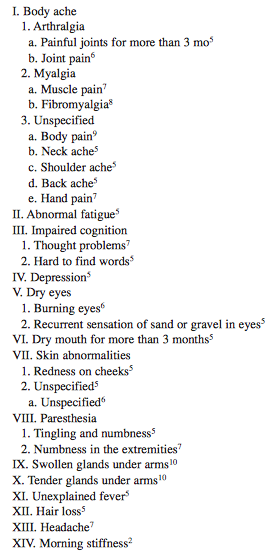
- Table 1. Symptoms/signs associated with rupture of silicone breast implant.
 Pleural silicone granuloma mimics pleural metastasis: Ruptured breast implant with silicone fistulising along a remote thoracotomy scar (2012). Link.
Pleural silicone granuloma mimics pleural metastasis: Ruptured breast implant with silicone fistulising along a remote thoracotomy scar (2012). Link.
- Silicone gel from ruptured implants can migrate to locations such as the chest wall, axillae, and upper extremities, resulting in granulomatous inflammation.
Soft, brown rupture: clinical signs and symptoms associated with ruptured PIP breast implants (2014). Link.
- Preoperative clinical signs including acquired asymmetry, breast enlargement, fullness of the lower pole, decreased mound projection, and change in breast consistency could be indicative of implant rupture.
- Device failure correlates with a low preoperative Baker grade of capsule.
- Brown-stained implants are more prone to implant failure.
- The presence of iodine in the gel suggests unacceptable permeability of the shell early in the implant’s life span.
Rupture and Intrapleural Migration of a Cohesive Silicone Gel Implant After Augmentation Mammoplasty: A Case Report (2011). Link.
- A 23-year-old female had received augmentation mammoplasty at a local clinic a week before visiting our hospital. When the patient’s doctor performed a breast massage on the sixth postoperative day, the left breast became flattened. The doctor suspected a breast implant rupture and performed revision surgery.
- The implant, however, was not found in the submuscular pocket and no definite chest wall defect was found in the operative field. The doctor suspected implant migration into the pleural cavity
- A CT scan revealed the ruptured implant in the left pleural cavity and passive atelectasis.
Cutaneous silicone granuloma mimicking breast cancer after ruptured breast implant (2011). Link.
Intrapulmonary and cutaneous siliconomas after silent silicone breast implant failure (2009). Link.
Silicone breast implant rupture presenting as bilateral leg nodules (2009). Link.
Peripheral blood eosinophilia, hyperimmunoglobulinemia and fatigue: possible complications following rupture of silicone breast implants (1996). Link.
Silicone Breast Implant and Automatic Implantable Cardioverter Defibrillator: Can They Coexist? A Case Report (2016). Link.
- We present a case of a silicone breast implant rupture after insertion of an automatic implantable cardioverter defibrillator (AICD).
Massive inflammatory reaction following the removal of a ruptured silicone implant masking the invasive breast cancer – case report and literature review (2016). Link.
An unusual case of a ruptured Poly Implant Prothèse breast implant associated with xanthoma (2016). Link.
Locoregional silicone spread after high cohesive gel silicone implant rupture (2006). Link.
- High cohesive gel implants may not be as safe as is commonly believed and all implant ruptures, irrespective of the cohesiveness of the silicone gel, should be investigated thoroughly.
Silicone gel breast implant rupture, extracapsular silicone, and health status in a population of women (2001). Link.
- Women with extracapsular silicone (silicone gel outside of the fibrous scar that forms around breast implants) were more likely to report having fibromyalgia or other CTD, which included dermatomyositis, polymyositis, Hashimoto’s thyroiditis, mixed CTD, pulmonary fibrosis, eosinophilic fasciitis, and polymyalgia than other women in the study.
Analysis of Risk Factors Associated with Rupture of Silicone Gel Breast Implants (1999). Link.
- Significant risk factors for breast implant rupture were identified: older implants, retroglandular implant location, implant contracture, local symptoms, certain implant type, and certain manufacturer.
How implants rupture according to Dr. Blais. Link.
Dr. Blais on rupture phenomena in implants, click here and scroll to page 10.
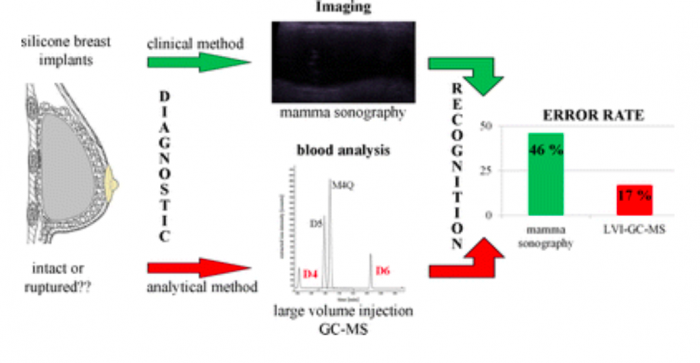
Cyclic volatile methylsiloxanes in human blood as markers for ruptured silicone gel-filled breast implants (2016). Link.
I just had an ultrasound and the results were BI-RADS category 2: Benign. I’ve been experincing some discomfort in my left breast. Itching close to armpit, rippling and sometimes little bit of numbness sensation. Should I be concerned about possible implant ruptured? Should I get an MRI? I want to mention that I just wean my baby (4months ago). Would like to explant next year, but im concern now that my implant can be ruptured